Science and Technology Daily: How Can Stem Cells Help Fight the Pandemic?
2020-03-05
Stem cells are multipotent cells with the remarkable ability to self-replicate and differentiate. Under specific conditions, they can give rise to various types of tissue cells, effectively replacing aging or dying cells. Moreover, stem cells secrete growth factors and cytokines that help regulate and enhance the body’s overall vitality—such as promoting angiogenesis, stimulating cell proliferation and differentiation, and even modulating inflammatory responses.
Currently, the battle against the pandemic has entered a critical phase. Given the urgent need for effective disease control, drug development is clearly one of the "main priorities."
Recently, at a press conference held by the State Council's Joint Prevention and Control Mechanism on science and technology innovation supporting COVID-19 control, Vice Minister of Science and Technology Xu Nanping announced that, in addition to traditional Chinese medicine, chloroquine phosphate, and convalescent plasma—already included in treatment protocols—drugs like favipiravir, remdesivir, and stem-cell therapy are also currently undergoing clinical trials. Notably, four critically ill patients who received stem-cell treatment have already been discharged from the hospital, and clinical trials will now be expanded further.
Since the onset of the pandemic, stem cell technology—often hailed for its "repair" and "renewal" capabilities—has captured widespread public attention. So far, what progress has been made in stem cell research aimed at treating COVID-19? And how exactly do stem cells work?
Targeting the epidemic, multiple key research projects have been launched.
Stem cells are multipotent cells with the unique ability to self-replicate and differentiate, capable of transforming into various specialized cell types under specific conditions. A growing body of research demonstrates that stem cells can differentiate in multiple directions, replacing aging or dying cells in tissues. Moreover, stem cells possess robust secretory functions, enabling them to release growth factors and cytokines that help regulate and enhance the body's overall vitality—for instance, by promoting angiogenesis, stimulating cell proliferation and differentiation, and even modulating inflammatory responses.
Stem cell technology has already been clinically applied to treat infectious diseases and their associated complications. Previously, researchers even experimented with stem cell therapy in the treatment of H7N9 avian influenza—and the results were highly promising. As a result, several medical and research institutions across China have now launched studies focused on using stem cells to combat COVID-19.
The Innovation Institute of Stem Cells and Regenerative Medicine at the Chinese Academy of Sciences develops CAStem, a new cell-based therapeutic drug.
According to the official website of the Ministry of Science and Technology, the Innovation Academy for Stem Cells and Regenerative Medicine under the Chinese Academy of Sciences has independently developed a novel cell-based drug called CAStem, which has demonstrated promising results in preliminary animal studies. The research team has now submitted an application for emergency approval to the National Medical Products Administration and is collaborating with relevant medical institutions. With approval from the ethics committee, clinical observation and evaluation are currently underway.
Clinical Study on the Safety and Efficacy of Mesenchymal Stem Cell Therapy for Patients with Pneumonia Caused by the 2019 Novel Coronavirus Infection
The team led by Academician Wang Fusheng from the Fifth Medical Center of the PLA General Hospital, in collaboration with Wuhan Jinyintan Hospital, Tianjin Haihe Hospital, and other institutions, is currently conducting a clinical study titled "Safety and Efficacy of Mesenchymal Stem Cell Therapy for Patients with Pneumonia Caused by the 2019 Novel Coronavirus Infection," recruiting patients to test the therapeutic potential of mesenchymal stem cells.
Zhejiang University First Hospital is preparing to use stem cell therapy for critically ill patients with the novel coronavirus.
Huang Jianrong, Deputy Director of the National Key Laboratory for Diagnosis and Treatment of Infectious Diseases, member of Zhejiang Province's Expert Group on Novel Coronavirus Pneumonia Prevention and Control, and Deputy Director of the Department of Infectious Diseases at the First Affiliated Hospital of Zhejiang University School of Medicine, also stated in a media interview that the First Affiliated Hospital of Zhejiang University has already completed discussions with its Ethics Committee and is preparing to apply stem cell therapy to severe cases of the novel coronavirus.
Professor Zuo from Tongji University School of Medicine leads the research team: Universal Lung Stem Cell Therapy Technology
Professor Zuo from Tongji University School of Medicine and his research team have been leveraging high-throughput single-cell sequencing technology for days, analyzing more than 43,000 lung cells in an effort to develop a versatile lung stem cell therapy that could be widely applied in the fight against the pandemic. Notably, the project has now entered the relevant regulatory review process and is expected to advance into the clinical phase in the near future.
In addition, several emergency science and technology projects focusing on stem-cell therapy for novel coronavirus pneumonia have been approved and are currently undergoing ongoing research and testing.
Faced with the novel coronavirus, researchers and medical professionals have responded swiftly, dedicating significant human and material resources. As a result, stem cell technology is emerging as one of the promising tools in the fight against the pandemic. Currently, multiple institutions are simultaneously advancing their research and development efforts, gradually moving into clinical trials to evaluate safety and efficacy. While progress varies across different projects, all are steadily working toward the same overarching goal.
How the coronavirus damages human lung tissue
After entering the body, the novel coronavirus gains access to cells by recognizing and binding to the ACE2 receptor on the surface of human cells. Once inside, the virus "hijacks" the cell's machinery to replicate its genetic material—RNA—and produce the proteins needed to form its protective outer shell. These components are then assembled into complete viral particles, which eventually cause the host cell to burst open, releasing the newly formed viruses to infect neighboring cells. This process triggers a robust inflammatory response, leading to severe damage in the lungs. The progression of COVID-19 can be clearly observed through dynamic changes captured in CT imaging.
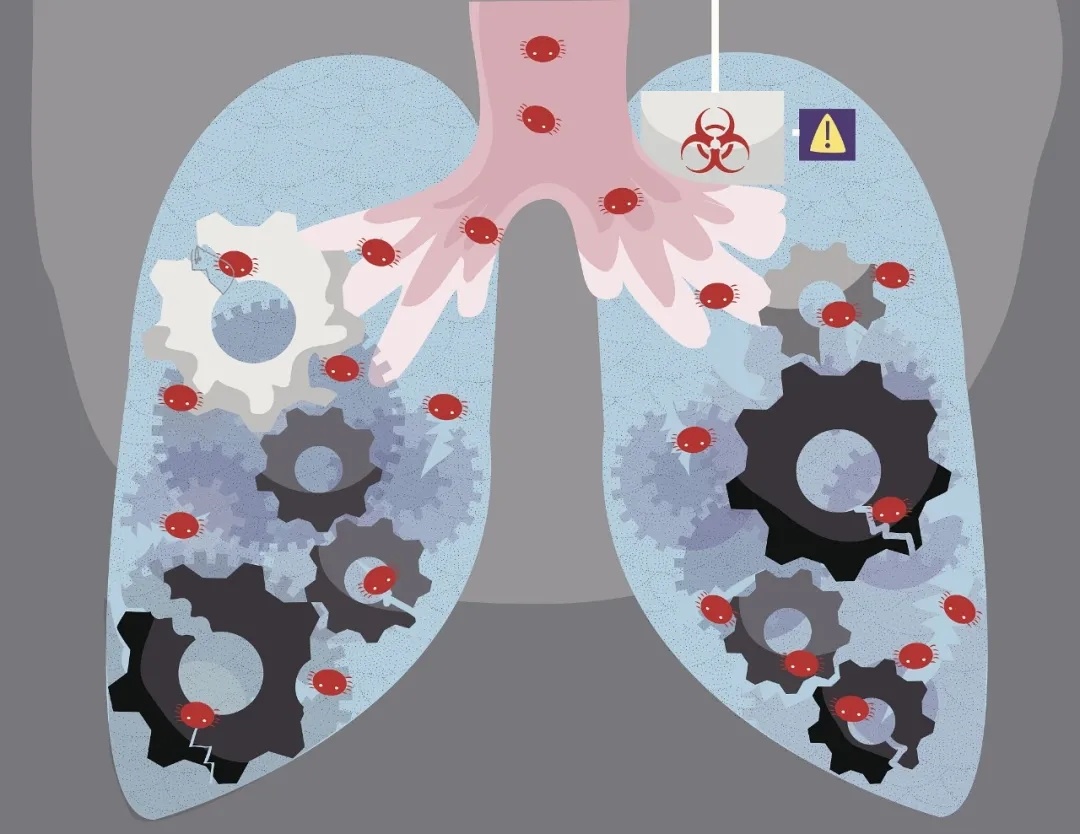
Image courtesy of Visual China
How stem cell therapy works to treat COVID-19
Research on stem cell technology as a tool to combat the pandemic is currently in full swing. But how exactly do stem cells play a role in treating COVID-19? And are there specific patient groups that would benefit most from this approach?
The Science and Technology Daily reporter, armed with the above questions, interviewed Zuo Wei. As the chief scientist of the National Key R&D Program’s “Stem Cells and Translational Research” project, he has long been dedicated to studying lung stem cells and is currently leading the research on the universal lung stem cell project aimed at combating COVID-19 mentioned earlier.
"At this stage, stem cell research focused on combating the pandemic is primarily centered on improving the conditions of critically ill patients," said Zuo Wei. He added that many people mistakenly believe that treating pneumonia often involves prioritizing antiviral strategies—aiming to eliminate the virus as quickly as possible. However, in reality, by the time a patient’s condition progresses to severe illness, the viral activity within their body has typically already dropped significantly. Instead, what truly drives the deterioration—or even death—in these patients is the overactivation of the body’s immune system triggered by the viral infection, leading to a "cytokine storm." This, in turn, causes inflammatory tissue damage in the lungs and impairs the lungs’ ability to efficiently exchange gases. Critically ill patients may also develop respiratory failure or acute respiratory distress syndrome. As Zuo Wei pointed out, lung inflammation and damage are currently the most pressing concerns for severely affected patients."
Lung tissue damage puts critically ill patients at risk of death, long-term complications, and other serious consequences. Stem cells are being widely regarded as holding great promise in repairing lung injuries in these patients.
Specifically, everyone’s body naturally retains a certain number of stem cells, and combating acute pneumonia relies primarily on bronchial basal cells— a type of lung stem cell. The lungs are a complex organ composed of the trachea, bronchi, and alveoli. When the lungs suffer extensive damage, the bronchial basal cells located in the bronchi migrate to the injured alveolar regions, effectively forming a "barrier." This barrier not only helps block off immune-inflammatory cells but also gradually matures into new alveoli over time.
Zuo told a reporter from Science and Technology Daily that, at this stage, the stem cells primarily used in COVID-19 treatment research fall into three main categories: mesenchymal stem cells, lung stem cells, and embryonic stem cells. Researchers typically administer these stem cell products via injection directly into the lungs of animal models or clinical trial participants.
"Under conditions free from external interference, if critically ill patients have highly active lung stem cells of their own, their lung function will recover more quickly and they’ll enjoy a better prognosis. Conversely, if their lung stem cells are less active, recovery will be slower and the prognosis poorer. That’s why we aim to protect and repair the lungs by supplementing them with exogenous lung stem cells," said Zuo. He added that lung stem cells can directly differentiate into functional lung cells, while embryonic stem cells can also achieve this goal through appropriate induction methods. Although mesenchymal stem cells cannot be directly induced to form lung-functional cells, they still hold potential benefits by secreting various immunomodulatory factors."
Although the mechanisms by which these three play a role in clinical settings differ, they can generally be summarized into two key functions: controlling inflammation and repairing damaged tissue. Stem cells achieve this by secreting anti-inflammatory factors that help restore the immune microenvironment in the lungs, thereby reducing the risk of lung failure caused by cytokine storms. Additionally, stem cells possess the remarkable ability to self-renew and differentiate, enabling them to generate specialized functional cells and regenerate alveoli—the critical structures responsible for gas exchange. This process ultimately promotes tissue repair and helps reverse pulmonary fibrosis, improving overall lung function.
Reprint Statement: This article is reprinted from Science and Technology Daily.
Related News




