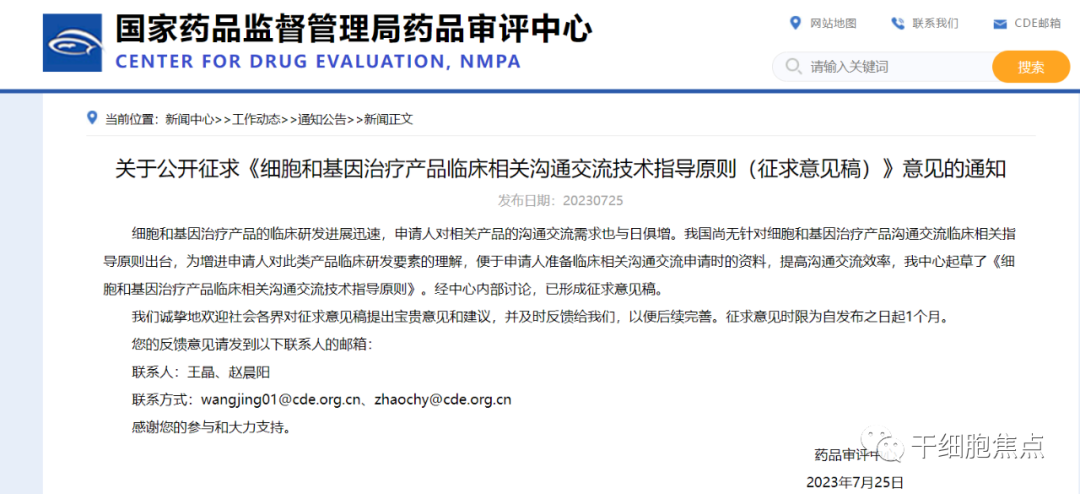
The Center for Drug Evaluation of the National Medical Products Administration has released the "Technical Guidance Principles for Clinical Communication and Exchange on Cell and Gene Therapy Products (Draft for Comments)."
2023-07-26
On July 25, 2023, the Center for Drug Evaluation of the National Medical Products Administration released the "Technical Guidance Principles for Clinical Communication and Exchange on Cell and Gene Therapy Products (Draft for Comments)." The main content of this guideline is divided into four sections: an overview, key considerations for communication, important notes, and examples. This guideline applies to communication regarding cell and gene therapy products based on clinical trial protocols. The deadline for submitting comments is one month from the date of publication.
The full text is as follows:
I. Overview
(1) Preface
In recent years, with continuous advancements in the scientific theories, technological approaches, and clinical practices related to cell and gene therapies, coupled with the gradual refinement of regulatory policies, the clinical development of cell and gene therapy products has experienced rapid and robust growth. Currently, several cell and gene therapy products—covering a diverse range of therapeutic types—have already been approved and launched globally. Domestically, CAR-T therapies targeting malignant hematological tumors have also entered the market. Meanwhile, numerous other cell and gene therapy products aimed at treating various indications are either advancing toward regulatory approval or have already moved into pivotal/confirmatory clinical trials. Additionally, many more innovative cell and gene therapy candidates—spanning a wide array of applications—are currently in various stages of clinical testing or are poised to initiate registration-enabling clinical trials. As a result, clinical-related communication and collaboration around these cutting-edge therapies have been steadily increasing.
Cell and gene therapy products differ from traditional small-molecule or large-biologic drugs, as their design and manufacturing processes may involve complex steps such as cell collection, ex vivo culture and expansion, isolation and purification, activation, or the selection of vectors, genetic modification, and genome editing—often evolving and being updated in tandem with advances in related research theories and technologies.
The personalized and unique nature of cell and gene therapy products inherently determines that their mechanisms of action, in vivo metabolic profiles, therapeutic outcomes, and adverse reactions all exhibit distinct characteristics. Moreover, the intricate design and complex manufacturing processes of these therapies, coupled with the integration of cutting-edge technologies, not only open up innovative treatment approaches and offer fresh therapeutic strategies but also potentially introduce heightened safety risks. To identify the optimal development pathway for such products while ensuring thorough assessment and effective management of both known and emerging risks, it is essential to tailor specific clinical research plans, trial protocols, and risk-management strategies to the unique attributes of each product. Given the distinctive features of cell and gene therapies, the design and execution of critical elements in clinical studies require careful attention—particularly during preclinical planning and throughout the course of clinical trials. Key considerations include product-specific characteristics, clinical positioning, target patient populations, dosing regimens, and study design. This guidance primarily addresses these factors, along with general considerations for ongoing communication and collaboration at various stages of development. As for the overarching principles governing drug clinical trials—and given overlaps with other guidelines—these will not be revisited in detail within this document.
(II) Purpose and Scope of Application
This guideline applies to cell- and gene-based therapeutic products developed and submitted for registration in accordance with relevant pharmaceutical regulations such as the *Drug Administration Law of the People’s Republic of China* and the *Measures for Drug Registration*. The cell- and gene therapy products covered by these guidelines primarily include human-derived stem cells and their derived cell therapies, immune cell therapies, gene therapies, and other similar products.
This guideline aims to provide recommendations on preparing communication materials and considering key clinical development elements throughout the clinical research and development process for cell and gene therapy products, with the goal of enhancing communication efficiency and ensuring the smooth advancement of these innovative therapies.
This guidance provides recommendations and suggestions on technical issues related to clinical communication for cell and gene therapy products, but it carries no mandatory legal force.
This guideline reflects the current views and understanding of the pharmaceutical regulatory authority. As research into cell and gene therapies advances, more experience is gained, and policies evolve, the relevant content in this guideline will continue to be refined and updated accordingly. Applicants are advised to promptly communicate with the Center for Drug Evaluation regarding the specific design and detailed aspects of their clinical studies involving cell and gene therapies.
II. Key Areas of Focus for Communication and Interaction
(1) The Purpose of Communication and Exchange During Key R&D Milestones
1. Pre-Application Communication for Clinical Trials
Before submitting the first clinical trial application, applicants should, in principle, submit a request for communication and exchange with the Center for Drug Evaluation to address critical technical issues prior to the initial submission. This step ensures that the clinical trial application documents are complete and that conducting the trial is feasible, all while prioritizing the safety of participants.
2. Pre-Initiation Consultation for Key/Confirmatory Clinical Trials
Key/confirmatory clinical trial pre-submission discussions will primarily focus on whether the existing research data sufficiently support the planned key/confirmatory clinical trial, as well as on reviewing and refining the trial protocol. Applicants may also provide a preliminary overview of their plans and strategies for regulatory submission.
3. Pre-Submission Communication and Consultation
According to the relevant provisions of the "Administrative Measures for Communication and Exchange in Drug Research and Development and Technical Review," applicants for marketing authorization of therapeutic biological products are, in principle, required to submit a request for communication and exchange to the Center for Drug Evaluation prior to filing their application. In cases involving conditional approval and/or applications eligible for priority review and approval procedures, applicants must first confirm these arrangements through communication and exchange with the Center before submitting their marketing authorization application to the National Medical Products Administration. The primary focus will be on evaluating whether the existing research data meet the technical requirements for drug marketing authorization.
(II) Key Projects for Communication and Exchange
1. Basis for the Proposed Study
Generally, it should include: the product's design principles, the therapeutic mechanism of action, an overview of the target indications, as well as the potential clinical benefits and clinical positioning of this product within those target indications. The analysis and elaboration of the rationale behind the proposed study are typically submitted during pre-clinical trial application discussions, and the product’s clinical positioning and key advantages continue to be refined throughout the product development process.
1.1 Principles of product design and mechanisms of therapeutic action
Since cell and gene therapy products involve novel principles and cutting-edge technologies in areas such as preparation, manufacturing, and treatment approaches—and because these products are currently classified as innovative drugs—there are significant differences in their therapeutic mechanisms across various product types. Even within the same product category, variations can exist. Therefore, providing a detailed explanation of the product’s design principles and its underlying mechanisms of action is essential for clearly highlighting its unique therapeutic features and advantages. Before submitting a clinical trial application, applicants should first offer a comprehensive overview and rationale behind the product’s design and its proposed mechanism of action, accompanied by relevant non-clinical study data. This ensures that the product has been rigorously developed and prepared, laying a solid foundation for future clinical trials by demonstrating both reliable safety and efficacy profiles.
1.2 Overview of the Target Indication and the Product’s Potential Clinical Advantages and Clinical Positioning in the Target Indication
Applicants must select the appropriate trial population and study design based on the product’s clinical positioning. For instance: If the product is intended to address the lack of effective treatment options following tumor recurrence, the trial typically enrolls patients with advanced, end-stage tumors who have already undergone standard therapies. In such cases, the clinical trial design could involve either a single-arm or randomized controlled approach. Alternatively, if the planned trial population includes patients who have received standard treatments, eligibility criteria can be defined by referring to current诊疗 guidelines—or by drawing insights from recent clinical trials of drugs approved for the same indication. The trial should then adopt a randomized, blinded design with parallel comparison to standard therapy, provided it is feasible.
An overview of the target indication may include, but is not limited to: the disease definition, pathogenesis, and epidemiological profile (e.g., regional distribution, temporal trends, and population demographics); disease subtypes/staging; commonly used diagnostic criteria and methods for assessing efficacy; standard treatment approaches currently available; and unmet clinical needs.
Before submitting the clinical trial application, it is also recommended to provide a concise summary of the research and development progress of similar products. Based on your understanding of existing treatments and comparable products, conduct a comparative analysis highlighting the product’s unique features and potential advantages, helping you initially define its clinical positioning. As the clinical study progresses, further insights into the safety and efficacy of the drug in the target population can be gathered through subgroup analyses and sensitivity assessments of the study participants. These findings can then inform discussions during pre-initiation communication with regulatory authorities regarding refined patient eligibility criteria for the upcoming pivotal or confirmatory clinical trials.
2. Clinical Development Plan and Clinical Trial Protocol
Applicants are encouraged to submit a more comprehensive clinical development plan and clinical trial protocol during pre-submission discussions for clinical trial applications. This practice will help regulatory agencies better understand the specific questions applicants raise regarding the clinical development plan and trial design, thereby fostering effective communication. Additionally, when initiating key/confirmatory clinical trials, applicants should scientifically design the proposed study protocols based on the analytical data from completed trials, ensuring that the submitted plans are both detailed and feasible.
2.1 Basic Content
Clinical research and development plans are typically formulated based on non-clinical study results and informed by the progress of similar product developments. They may include, but are not limited to: a product overview, an overall R&D plan (which must at least cover the proposed indications, preclinical evaluations, clinical assessments where applicable, R&D strategies, the clinical development pathway, and outlines of study designs and protocols for each phase), as well as a project timeline. Additionally, clinical trial protocols must be scientifically sound, comprehensively detailed, and practically feasible. Key components should include at least the trial title (including protocol number, version number, and version date), study objectives, trial design, target population (inclusion and exclusion criteria), dosing regimen, sample size, primary endpoints, and the overall trial procedure.
2.2 Key Factors in Clinical Trial Design
The design of a clinical trial protocol must align seamlessly with the product’s scientific rationale and its intended clinical positioning. For instance, the selection of the trial population and the study design should precisely meet the requirements needed to achieve the research objectives. Additionally, the choice of primary endpoints should effectively reflect the clinical needs of the target population as well as the unique characteristics—or even advantages—of the product. In early-stage exploratory clinical trials, the primary endpoint typically focuses on evaluating the product’s safety. Given that the safety risks associated with certain cell- and gene-based therapies remain unclear—particularly for gene-edited cells and gene-editing products—it is strongly recommended that applicants pay close attention during pre-trial discussions to key aspects of the protocol, such as the safety monitoring criteria and the definition of dose-limiting toxicity (DLT) during dose-finding phases. Importantly, the DLT definition should be tailored specifically to the product’s unique design, carefully balancing its distinct features in a scientifically sound manner—rather than simply adopting standards from other similar products.
Given that cell and gene therapy products operate through mechanisms distinct from traditional treatments—primarily by addressing the root cause of diseases—it is crucial to carefully select efficacy endpoints in evaluating these products, ensuring they simultaneously capture both clinical benefits and the therapeutic advantages tied to treating the underlying cause. We recommend thoroughly exploring potential efficacy metrics during early-stage exploratory clinical trials, providing a solid foundation for identifying appropriate endpoints in later, larger-scale clinical studies.
Applicants must select the appropriate trial population and study design based on the product’s clinical positioning. For instance: If the product is intended to address the lack of effective treatment options following tumor recurrence, the trial typically enrolls patients with advanced, end-stage tumors who have already undergone standard therapies. In such cases, the clinical trial design could involve either a single-arm or randomized controlled approach. Alternatively, if the planned trial population includes patients who have received standard treatments, eligibility criteria can be defined by referring to current诊疗 guidelines—or by drawing insights from recent clinical trials of drugs approved for the same indication. The trial should then adopt a randomized, blinded design with parallel comparison to standard therapy, provided it is feasible.
When developing inclusion and exclusion criteria for clinical trial protocols, it’s important to pay close attention to cell and gene therapy products that carry higher-than-expected risks and/or involve more unknown risks. For these products, it’s crucial to define specific, clear-cut indicators—for example, clearly specifying the number of prior lines of therapy based on the current state of diagnosis and treatment for the targeted indication, as well as precisely outlining what constitutes "adequately treated" in each therapeutic line. Currently, the definition of "adequate treatment" typically requires either a sufficiently long (complete) treatment course—or an explanation for why a full course couldn’t be completed, such as the patient’s intolerance to treatment-related toxicities. Importantly, any determination of "intolerance" must be supported by objective, verifiable evidence.
The dosing regimen typically includes the route of administration, dosage amount, dosing interval, number of doses, and treatment duration. Given the unique characteristics of cell and gene therapy products, non-clinical studies may have limited value in guiding the development of an appropriate dosing regimen. Therefore, applicants are advised to carefully and scientifically formulate the dosing plan, drawing on both non-clinical data and completed clinical studies of similar products as a reference.
The clinical trial protocol submitted during the pre-initiation meeting for a pivotal/confirmatory clinical trial must build upon the exploratory phase by further defining the characteristics of the intended confirmatory patient population, refining the key inclusion and exclusion criteria, selecting an appropriate dosing regimen, clearly specifying or adjusting, as needed, the primary and secondary efficacy endpoints, outlining critical safety considerations, and explicitly stating the statistical hypotheses in alignment with the study objectives.
At this stage, applicants need to not only focus on selecting the appropriate efficacy endpoint metrics but also clearly define the criteria for evaluating efficacy, as well as specify the requirements for evaluators. Depending on the specific disease and its efficacy assessment standards, the protocol should explicitly outline the timing of efficacy evaluations and any associated requirements for confirming these assessments (where applicable).
To further clarify the clinical positioning, applicants must carefully consider and select an appropriate clinical trial design when developing pivotal/confirmatory trial protocols. If a randomized, blinded, controlled trial is planned, key considerations should include the selection of the control drug and the formulation of statistical hypotheses. The choice of the control drug must align with the product’s intended clinical indication and reflect the current standard of care for the targeted condition. In the clinical development of certain novel cell and gene therapy products—given their potentially higher safety risks—applicants may opt for a single-arm trial design in pivotal/confirmatory studies. To ensure that such single-arm trials can generate the necessary safety and efficacy data required for regulatory approval, applicants are advised to clearly define the statistical hypotheses underlying efficacy assessments within the pivotal/confirmatory trial protocol and specify the target sample size needed for the study. Additionally, the efficacy threshold chosen for the single-arm trial must be rigorously justified, while the required number of participants should not only meet the statistical hypothesis calculations but also allow sufficient time for comprehensive safety risk evaluations.
3. Risk Management Plan
A risk management plan typically includes a pharmacovigilance activity plan and risk control measures. Applicants should, while complying with China’s pharmaceutical regulatory laws and regulations, also refer to relevant ICH guidelines and technical guidance principles issued by China’s drug regulatory authorities to finalize the product’s pharmacovigilance activity plan. Given that, prior to clinical trial approval, the product may still lack clinical safety data, applicants must thoroughly analyze the completed non-clinical study data and draw on known safety risks associated with similar products. Based on the product’s specific characteristics, they should develop a comprehensive overview of drug safety along with detailed risk management strategies. During the pre-approval communication phase for clinical trials, it’s crucial to refine the mechanisms for revising the clinical risk management plan, ensuring that once clinical trial data become available, the plan can be updated promptly and effectively. Additionally, during key/confirmatory clinical trial initiation discussions and pre-marketing application communications, applicants are required to submit an updated clinical trial risk management plan—refined based on clinical trial results—or, alternatively, a post-marketing risk management plan formulated from the clinical trial safety summary. It’s important to note that the risk management plan is an evolving process: as clinical development progresses, the overall safety profile of the product becomes increasingly clear.
4. Summary of Completed Clinical Trials
During pre-critical/confirmatory clinical trial and pre-marketing authorization communication sessions, applicants must submit at least the results of completed clinical trials.
During pre-communication for pivotal or confirmatory clinical trials, applicants are required to provide a concise summary of the completed clinical studies. They should analyze whether the results from this phase have met the objectives outlined in the overall development plan, and conduct an initial assessment of the product’s benefit-risk profile. Additionally, applicants must evaluate whether and how the available data support the initiation of the pivotal/confirmatory trial. This evaluation can be informed by summarizing and analyzing the data from prior clinical trials, allowing for a thorough assessment of the safety and efficacy of the dosing regimen as originally proposed. Such analysis will help determine critical information about dose-safety and dose-effect relationships. Applicants may also examine the demographic characteristics of participants in earlier trials—such as age, gender, occupation, race/ethnicity, behavioral traits, marital status, and more—to identify specific subgroups that demonstrated a favorable benefit-risk profile following treatment. These insights will serve as valuable guidance for further refining the optimal dosing strategy and identifying the most appropriate patient population for the intended indication. Lastly, while summarizing the findings from previous clinical trials, applicants should assess whether the initially selected efficacy endpoints effectively captured meaningful clinical benefits for patients. They should also determine which specific outcome measures showed the most pronounced improvements among treated participants, providing a clearer picture of the therapy’s therapeutic impact.
During pre-approval communication with regulatory authorities, applicants are required to submit, whenever possible, the complete clinical trial reports for pivotal/confirmatory studies, along with the clinical trial protocol and its revision history, including reasons for each amendment. Additionally, applicants should provide the statistical analysis plan and closely monitor whether the execution of the pivotal/confirmatory trial aligns with the consensus reached during the pre-trial discussions. Key areas of focus include, but are not limited to: ensuring that the eligible patient population matches the agreement made during the pre-trial discussions—particularly in terms of disease type and prior treatment history; detailing how many subjects were actually screened and enrolled against the inclusion/exclusion criteria; providing comprehensive information on cases where screening failed or subjects withdrew from the study, to avoid any potential bias in subject selection; verifying that the statistical analysis datasets are appropriately defined, and confirming whether the number of cases in the efficacy and safety datasets meets the agreed-upon thresholds discussed during the pre-trial talks. It’s also crucial to ensure that all subjects included in the efficacy and safety datasets have completed the relevant endpoints for evaluation. Furthermore, assess the appropriateness of the efficacy assessment criteria and compare them with the standards outlined during the pre-trial discussions. Conduct thorough sensitivity analyses to evaluate their rationale and robustness. Finally, ensure that safety data collection and reporting are conducted in full compliance with regulatory requirements, and provide detailed analyses of SAEs, prioritized adverse events, and fatal outcomes. Additionally, thoroughly evaluate and explain any newly identified safety risks.
5. Other
When submitting an application for clinical-related communication regarding cell and gene therapy products, applicants should note that, due to the unique nature of these products, pharmacological and non-clinical study data may cover aspects such as product safety, clinical safety risks, and risk management strategies—and relevant documentation must also be provided. During pre-communication meetings ahead of pivotal or confirmatory clinical trials, applicants are encouraged to briefly outline their plans and strategies for regulatory submission. Depending on the specific submission plan or strategy, the design of key factors in the pivotal/confirmatory trial may vary significantly. For instance, if the goal is to seek either full approval or conditional approval for market launch, the statistical analysis plan, selection of primary endpoints, and determination of follow-up durations in the pivotal trial may require distinct considerations.
(III) Special Considerations for Communication and Interaction with Different Cell and Gene Therapy Products
1. Human-derived stem cells and their cell-derived therapeutic products
Human-derived stem cell–derived cell therapy products refer to cellular therapies obtained by inducing differentiation from human-derived stem cells (including human embryonic stem cells, adult stem cells, and induced pluripotent stem cells) or by directly reprogramming mature somatic cells into functional cell types. Given the diverse cellular origins of human-derived stem cells and their corresponding cell therapy products (hereinafter referred to as "stem cell-related products"), applicants are required to provide detailed information—such as the source and preparation methods—during pre-clinical trial communication and review, along with a thorough analysis of the product’s ethical risks, to determine whether clinical trials in humans can proceed. For stem cell clinical research projects that have already been registered in accordance with the "Provisional Measures for the Administration of Clinical Research on Stem Cells" and are now being considered for drug registration applications, applicants must submit the registered study design, protocols, and results during pre-trial communication. Additionally, they should clearly demonstrate how the previously conducted registered studies support the development of critical elements for subsequent research planning and clinical trial designs.
Since the therapeutic mechanisms of current stem cell-related products often rely on functions such as cell distribution, engraftment, proliferation, and secretion, the conditions they target are mostly non-life-threatening diseases. Clinically, the primary goals of treatment typically focus on symptom relief and disease progression delay. Therefore, during trial design, it is essential to carefully consider—and promptly communicate with the Center for Drug Evaluation—key factors specific to clinical trials, such as: selecting either a monotherapy approach or adding the drug (combination therapy) based on the clinical setting; determining whether and at which trial stage a control group should be included; choosing an appropriate comparator drug; and deciding on the selection of clinical endpoints for different trial phases.
Stem cell-related products may involve genetic modifications. Currently, the primary goals of gene editing in stem cells include enhancing their expansion and differentiation capabilities, as well as reducing immune rejection responses. Additionally, gene-editing tools are being used to integrate exogenous target genes into the stem cell genome, offering potential treatments for genetic disorders caused by gene function loss—such as congenital immunodeficiencies—and certain blood diseases. These genetically engineered stem cell-based products could significantly improve therapeutic outcomes while broadening the scope of diseases that can be treated with stem cell therapies. For instance, ongoing research includes projects aimed at repairing the IL2RG gene in hematopoietic stem cells (HSCs) to treat X-linked severe combined immunodeficiency type X; others focus on boosting patients' resistance to HIV by knocking out the CCR5 gene in HSCs; and yet others seek to activate γ-globin expression in HSCs by silencing the BCL11A gene, with the goal of treating sickle cell anemia and β-thalassemia. When discussing clinical development plans and trial protocols for these innovative products, it’s crucial to consider additional safety concerns arising from genetic modifications, such as the potential increase in tumorigenicity, uncontrolled proliferation, or unpredictable expression of introduced genes.
2. Immune cell therapy products
Immune cell therapy products are cellular treatments that utilize immune cells derived from either the patient themselves or a donor. These cells undergo processes such as ex vivo culture and expansion, activation, genetic modification, or gene editing, before being reintroduced into the patient’s body. By stimulating or enhancing the body’s immune system, these therapies aim to control disease progression. Currently, the primary cell types involved in immune cell therapies include T cells, natural killer cells (NK cells), dendritic cells (DCs), and others.
Immune cell therapy products are derived from adult immune cells, and the complex procedures involved in their ex vivo preparation, along with their survival mechanisms and modes of action within the body, can potentially increase safety risks in clinical applications. Moreover, different types of immune cell therapies may pose significantly varying safety risks depending on their specific application. Given the relatively high risk profile of immune cell therapies, the populations or patient groups selected for clinical trials—such as those with specific indications—are typically individuals who can tolerate higher treatment risks. However, due to stringent requirements related to the quality of starting cells (e.g., in autologous immune cell therapies, severely ill patients may lack the ability to provide suitable raw materials for preparation or produce cell products meeting regulatory standards), as well as constraints like prolonged preparation timelines and limitations on concomitant medications, rapidly progressing or critically ill patients may not be the optimal candidates for these studies. Therefore, when designing clinical trials, it’s crucial to carefully evaluate the potential benefits versus risks for the target population, ensuring that all stakeholders—including researchers, regulators, and patients—are fully informed about these considerations throughout the trial process.
Currently, gene-modified immune cell products primarily include chimeric antigen receptor T cells (CAR-T), chimeric antigen receptor NK cells (CAR-NK), T-cell receptor-engineered T cells (TCR-T), and tumor neoantigen-targeted T cells. Among these, the most common genetic modifications focus on enhancing T cells' ability to recognize tumor-specific antigens, thereby boosting their targeted killing of cancer cells. Additionally, these products may also incorporate genetic fragments that enable immune cells to express other small-molecule substances.
The gene-editing processes for these products are relatively complex, and the objectives of genetic modification vary widely, potentially posing safety risks such as tumorigenicity and uncontrolled expression of exogenous genes. When initiating communication and discussions, it’s essential not only to clearly outline the thorough safety assessments conducted prior to clinical trials but also to address the scientific rationale and appropriateness of the safety and efficacy evaluation metrics, as well as the follow-up timelines, used during the trials. For instance: Should monitoring for toxicity related to exogenous gene overexpression be included in the definition of Dose-Limiting Toxicity (DLT) during dose-escalation studies? How should monitoring schedules and specific indicators, along with criteria for discontinuation and mitigation strategies, be designed within the clinical trial protocol and risk management plans to address concerns like excessive cell proliferation and unintended exogenous gene expression? Additionally, what efficacy endpoints should be established, tailored specifically to the goals and advantages of the genetic modifications being tested?
For tumor neoantigen T-cell therapies and other genetically modified cell-based treatments that involve introducing exogenous genes into cells via big-data screening, it is crucial to thoroughly explain the methodology and rationale behind the data selection process during pre-clinical trial communication and consultation, ensuring the scientific rigor and robustness of the approach.
As CAR-T product research advances, allogeneic CAR-T products or in vivo–edited CAR-T products have either entered or are being submitted for clinical trials. In addition to addressing the aforementioned concerns during clinical trial communication and collaboration, it’s also crucial to pay close attention to combination therapies—specifically, the source and dosing of anti-CD52 monoclonal antibodies, as well as safety and efficacy considerations related to in vivo gene-editing technologies such as CRISPR/Cas9.
Immune cell therapy products may involve numerous personalized preparation steps. When communicating the clinical trial design for such products, it is crucial to pay special attention to issues like study population selection, concomitant medication use, bridging therapies, strategies for addressing preparation failures (including alternative rescue treatments, re-preparation procedures, and principles for subject replacement), as well as ensuring consistency throughout the preparation and administration processes.
3. Gene therapy products
Gene therapy products primarily include nucleic acids (e.g., plasmids, RNA), gene-modified microorganisms that express specific genes (e.g., viruses, bacteria), products designed for in vivo editing of the host genome—either with or without specific transcription/translation processes—and microorganisms that do not rely on genetic modification to express particular genes (e.g., oncolytic virus products).
These products can deliver exogenous genes into target cells via a vector, correcting or mitigating defects caused by disease-causing genes to achieve therapeutic effects. For instance, an appropriate vector—such as adeno-associated virus—can be used to carry the gene (or a fragment) encoding a clotting factor, enabling its expression within hemophilia patients and thereby boosting their levels of the essential clotting factor.
The risks associated with gene therapy products primarily stem from the gene vectors and the genes they carry. When initiating a communication and exchange, applicants must first conduct thorough research and exploration into the rationale and safety of the vector chosen for their product. Additionally, they should provide comprehensive explanations regarding the product’s gene-modification mechanism and the genes being delivered, enabling a robust assessment of the overall safety risks.
Gene therapy products come in a diverse range of types, and due to their differing modification mechanisms, they are expected to deliver varying therapeutic outcomes. Additionally, there are distinctions in the targeted indications, the patient populations they aim to treat, and the specific delivery methods used for each product. For instance: - Gene therapy for hemophilia typically involves intravenous infusion. - In contrast, gene therapies targeting age-related macular degeneration often employ subretinal, vitreal, or suprachoroidal injections. - For gene therapy using naked plasmid DNA to treat lower limb ischemia, local multi-point injection is commonly used—and this approach may require an electroporation system or device. When communicating with regulatory authorities, applicants must thoughtfully integrate the clinical needs of the target patient population with the anticipated benefits of gene therapy, while also proposing appropriate safety and efficacy evaluation metrics along with a comprehensive follow-up plan. For therapies requiring device-assisted delivery, applicants should clearly explain the device’s mechanism of action and provide detailed instructions for its use. Similarly, for treatments involving surgical delivery, applicants must justify the chosen administration method and outline precise procedural steps to ensure safe and effective implementation.
Gene therapy products are typically expected to deliver long-term therapeutic benefits, yet they may also introduce unpredictable risks, such as delayed adverse reactions. Therefore, applicants conducting clinical trials for gene therapy products must prioritize the assessment of these potential risks—particularly delayed adverse effects—and implement robust risk-mitigation strategies. It is advisable to discuss and identify risk factors that could lead to delayed adverse reactions during pre-submission discussions. Based on this analysis, applicants should develop a well-structured, long-term follow-up plan, carefully outlining specific milestones, duration, and key monitoring parameters. During the benefit-risk evaluation phase of the clinical trial application process, applicants should clearly articulate how the proposed long-term follow-up plan, comprehensive risk management strategy, and even draft informed consent documents address and mitigate these risks. As additional critical information about product safety emerges—whether during the clinical trial or post-marketing—it’s essential to promptly update relevant documentation. Furthermore, applicants may proactively seek further guidance or clarification on any emerging concerns through appropriate communication channels.
Cell and gene therapy products vary widely in type, involve complex mechanisms, and differ significantly in dosing regimens and patient populations for specific indications. When seeking communication and consultation, applicants are advised to tailor their discussions—focused on critical technical issues—to the unique characteristics of their product, while aligning with the objectives of clinical trials at each stage.
III. Important Notes
This section is primarily based on past communication and exchange experiences in the clinical field related to cell and gene therapy products.
(1) The Timing for Communication and Interaction
According to the *Drug Registration Management Measures*, the *Measures for Communication and Exchange in Drug Development and Technical Review (Trial)*, and their revision notes, applicants seeking conditional approval and/or those eligible for priority review and approval procedures must submit a communication and exchange request as required.
Applicants should pay special attention to the following points outlined in the "Notice of Approval for Clinical Trials": - "Before initiating the clinical trial, communicate and exchange information with the Center for Drug Evaluation regarding the clinical trial protocol." - "After completing the exploratory clinical trial, submit a request for communication and exchange with the Center for Drug Evaluation prior to launching the confirmatory (or pivotal) clinical trial, to ensure the subsequent trial protocol is thoroughly evaluated."
During other development stages in the clinical trial process, if there is a need for communication and exchange, stakeholders may submit requests in accordance with the "Administrative Measures for Communication and Exchange in Drug Development and Technical Review (Trial)."
Communication and consultation regarding pediatric medications can be conducted in accordance with the "Provisional Detailed Rules for Applying for and Managing Class I Meetings in Pediatric Medication Communication and Consultation."
(II) Preparation of Communication Materials
According to the relevant requirements of the "Administrative Measures for Communication and Exchange in Drug Research and Development and Technical Review," applicants should complete the drug's basic information and development status in the communication and exchange application form. For applications involving clinical trial protocols, detailed, actionable, and comprehensive clinical trial plans must be provided—based on the indication target—using the materials from the communication and exchange meeting as well as the clinical trial protocol itself, in alignment with the applicable regulatory standards for review and evaluation.
Given the highly innovative nature and rapid R&D progress of cell and gene therapy products, please also provide any additional relevant materials, such as previous discussions or communications regarding this product, updates (or summary reports) on clinical trials for other indications of this product, progress (or summary reports) from investigator-initiated clinical studies targeting the same indications, developments in similar products, or updates/clinical trial highlights from industry conferences and related publications—these can all serve as valuable references during our communication.
Cell and gene therapy products may be simultaneously submitted for registration to regulatory agencies in multiple countries or regions. Given factors such as differences in the racial characteristics of domestic and international subjects, variations in regulatory policies between domestic and foreign drug authorities, and considerations related to product manufacturing and supply, meeting minutes or records from discussions with regulators in other countries also serve as critical materials for communication with the Center for Drug Evaluation. Therefore, it is recommended that these documents be provided as well.
(III) Issues in Communication and Interaction
Communication issues should be clear, specific, and targeted—briefly outlining the context of the problem, clearly stating the purpose behind raising it, and presenting the applicant’s perspective along with supporting evidence. Avoid asking vague questions, such as: "Is the clinical trial protocol feasible?"
Questions regarding the key design elements of clinical trial protocols should be supported by appropriate evidence. For instance, when evaluating whether the dose selection for Phase I clinical trials of cell and gene therapy products is reasonable, in addition to providing preclinical study data, dose levels used in clinical trials of similar products also serve as an important reference. Similarly, for determining the rationale behind multiple dosing regimens in cell and gene therapies, factors such as immunogenicity and pharmacokinetic studies should be carefully considered, ensuring that the chosen number of doses and dosing intervals are well-justified.
(IV) The Discipline of Communication and Interaction
If applying for a pre-approval meeting regarding a confirmatory clinical trial protocol, it is recommended to simultaneously engage with both clinical and statistical experts to discuss key aspects such as the trial design and statistical hypotheses. In the application materials, please provide detailed and robust justification for the trial design and statistical assumptions. Particularly for cell and gene therapy products targeting advanced-stage tumors or rare diseases, an external-controlled, single-arm clinical trial design may be considered. In such cases, high-quality research literature on historical treatments or epidemiological data should be submitted as the basis for establishing the statistical hypothesis parameters.
Due to the complex manufacturing processes involved in cell and gene therapy products, pharmaceutical process optimization and changes may occur during clinical trials. If significant pharmaceutical changes arise during confirmatory clinical trials, it is recommended to simultaneously engage with experts from pharmaceutical sciences, pharmacology and toxicology, clinical disciplines, and statistics to discuss whether the comparability of these pharmaceutical changes requires clinical trial verification.
(5) Application for Communication and Exchange on Multiple Indications
Certain types of cell and gene therapy products have complex mechanisms of action, offering potential benefits for multiple indications that target the same pathway or share similar disease mechanisms. If the same product is intended to initiate clinical trial discussions for several distinct indications, it is recommended that separate communication requests be submitted for each indication.
(6) Forms of Communication and Interaction
The format of communication will depend on how best to address the issue at hand. If the applicant’s concern can be effectively resolved through written feedback, there will no longer be a need to hold face-to-face, video, or phone-based discussion meetings.
4. Examples
Through examples, the aim is to outline how to initiate communication and dialogue based on a given issue.
Basic information about the variety: A certain oncolytic virus is a conditionally replicating, recombinant oncolytic adenovirus engineered based on the serotype X adenoviral backbone.
Pharmaceutical background information: The original adenovirus promoter was replaced with a tumor-specific gene promoter to enable selective replication in cancer cells. Additionally, the native adenoviral backbone proteins were engineered to create a chimeric vector primarily based on Adenovirus serotype X, aiming to reduce immunogenicity, enhance the virus's ability to infect tumor cells, facilitate clearance from normal cells, and minimize hepatotoxicity. Finally, expression cassettes encoding cytokines and other therapeutic genes were incorporated to synergistically boost the anti-tumor efficacy.
Non-clinical background information: in vivo and in vitro pharmacodynamic studies, pharmacokinetic studies, toxicology studies, and more.
Communication and Exchange Application Stage: Before applying for a clinical trial
Subjects proposed for discussion and exchange: Clinical Specialty
Applicant submits documents: Application form for communication and exchange meetings, communication and exchange meeting materials, communication and exchange meeting PPTs, clinical development plans and early exploratory clinical trial protocols, risk management plans, clinical review reports, pharmaceutical review reports, non-clinical review reports, and other relevant documents.
One of the issues proposed for discussion and exchange: Is the definition of DLT reasonable?
Applicant's Perspective:
The applicant, referring to the DLT definition for similar products, has established an identical DLT definition for this product.
CDE Perspective: While the DLT definition for similar products can serve as one reference point for planning clinical studies, it is recommended that the DLT definition be developed scientifically by starting with the product’s own design and carefully considering its unique characteristics.
Recommended to follow:
(1) Product-specific features: ① Compared to similar products, the viral vector used in this product differs. While the reference product employs a serotype Y adenovirus vector, our product utilizes a genetically modified, chimeric adenovirus vector. Since chimeric vectors derived from other serotypes have seen limited research and application, it may be necessary to conduct the most comprehensive investigation possible into this structural modification. Additionally, given the potential differences in safety risks among various viral vectors, safety monitoring indicators related to vector-specific risks should be incorporated into the definition of DLT (Dose-Limiting Toxicity). ② This product incorporates genes encoding specific cytokines or other therapeutic factors into an oncolytic virus vector. Once cells are infected, they will begin expressing and secreting these cytokines, which could lead to unintended adverse reactions that require careful monitoring.
(2) Non-clinical animal toxicology studies revealed that the test animals exhibited acute liver and kidney dysfunction related to the test substance, leading to animal deaths. Notably, the original definition of Dose-Limiting Toxicity (DLT) did not include renal toxicity; therefore, it is recommended that this aspect be revised and clarified.
(3) DLT Observation Period. Based on the observation periods of similar products, the DLT observation period for this product has been set at 28 days. However, non-clinical study results indicate that adverse reactions may persist up to 41 days. Therefore, the DLT observation period should be reasonably adjusted by considering the timing of onset, duration, and resolution of relevant toxic effects observed in the non-clinical studies.
As this example demonstrates, the applicant has submitted fairly comprehensive documentation; however, they failed to clearly identify the key factors for the clinical trial based on their product’s specific characteristics and preliminary research data. This requires particular attention.
5. References: Omitted
6. Appendix: Omitted
Reprint Notice: This article is reprinted from the website of the Center for Drug Evaluation under the National Medical Products Administration. If there is any infringement, please contact us for removal.
Previous:
Related News




